The exact cause of eczema is unknown, but it is thought to be a combination of genetic, environmental, and immunological factors. Eczema symptoms can develop and worsen due to a variety of triggers and risk factors.
The following are the primary causes and factors associated with eczema:
- Genetics: Eczema tends to run in families, suggesting a genetic predisposition. If you have a family history of eczema or other atopic conditions (such as asthma or hay fever), you may be at a higher risk of developing eczema.
- Abnormal Immune Response: Eczema is considered an immune-mediated condition. Individuals with eczema may have an overactive immune response to certain triggers, leading to inflammation and skin irritation.
- Skin Barrier Dysfunction: People with eczema often have a compromised skin barrier, which makes their skin more susceptible to irritants, allergens, and infection. The damaged skin barrier allows moisture to escape and allergens to penetrate, leading to dry, itchy, and inflamed skin.
- Environmental Triggers: Exposure to certain environmental factors can exacerbate eczema symptoms. Common triggers include harsh soaps and detergents, irritating fabrics, extreme temperatures, low humidity, and exposure to allergens such as pollen, dust mites, pet dander, and mold.
- Allergies: Eczema and allergies are closely related, and individuals with eczema may have other allergic conditions, such as asthma or hay fever.
- Stress: Emotional stress can sometimes worsen eczema symptoms or trigger flare-ups in susceptible individuals.
- Microbial Infections: Bacterial, viral, or fungal infections can aggravate eczema, especially when the skin is scratched, leading to breaks in the skin barrier.
How is eczema diagnosed?
A healthcare provider will diagnose eczema after a physical exam, where they can take a close look at your skin. Most often, people receive an eczema diagnosis as a child, as it’s common among children, but a diagnosis can happen at any age when symptoms arise.
Symptoms of eczema can look similar to other conditions. Your provider might offer tests to rule out other conditions and confirm your diagnosis. Tests could include:
- An allergy test.
- Blood tests to check for causes of the rash that might be unrelated to dermatitis.
- A skin biopsy to distinguish one type of dermatitis from another.
What questions might my healthcare provider ask to diagnose eczema?
Your healthcare provider might ask the following questions to learn more about your symptoms, including:
- Where do you have symptoms on your body?
- Did you use any products to try to treat your skin?
- Do you have any medical conditions like allergies or asthma?
- Do you have a history of eczema in your family?
- How long have you had symptoms?
- Do you take hot showers?
- Is there anything that makes your symptoms worse?
- Have you noticed something triggers or worsens your symptoms like certain soaps or detergents?
- Do your symptoms affect your ability to sleep or perform your daily activities?
Who diagnoses eczema?
A primary care provider may recommend you visit a dermatologist to diagnose and treat your eczema. A dermatologist specializes in skin conditions.
MANAGEMENT AND TREATMENT
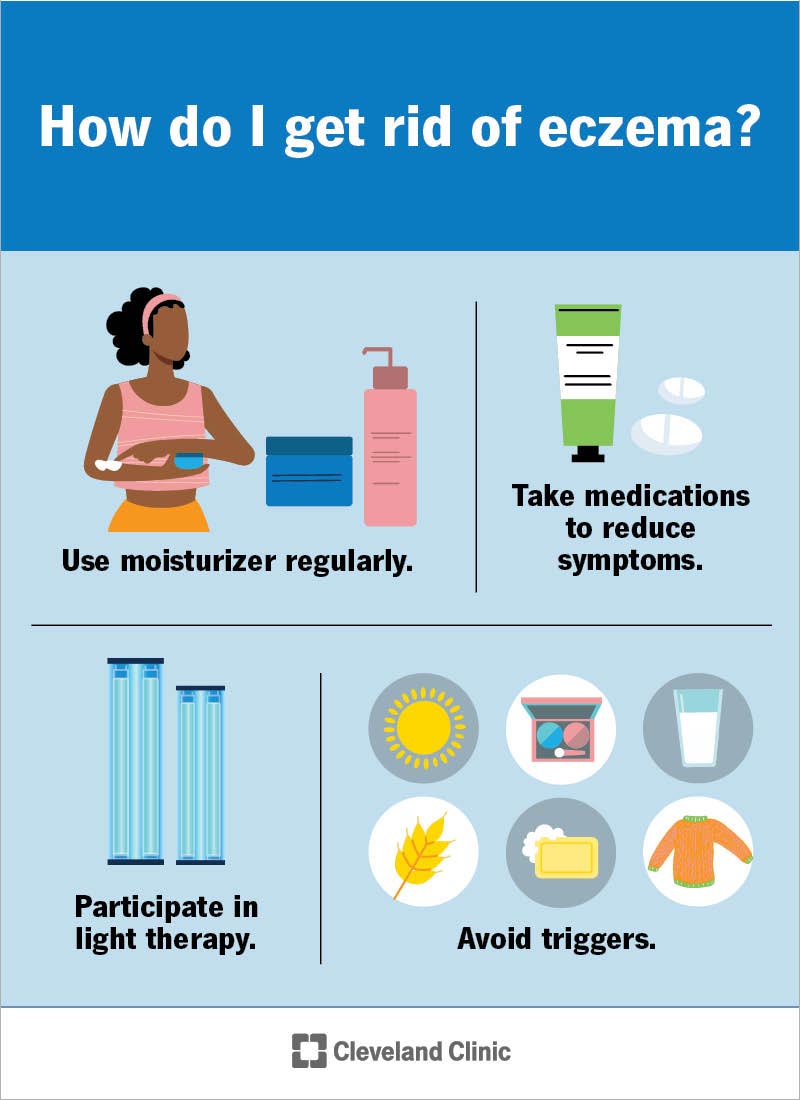
How do I get rid of eczema?
Your treatment for eczema is unique to you and what caused your symptoms to flare up. Treatment for eczema could include:
- Using gentle or sensitive skin moisturizers throughout the day when you have dry skin. Apply moisturizer when your skin is damp after a bath or shower.
- Apply topical medications to your skin as advised by your provider, like topical steroids.
- Take oral medications like anti-inflammatory medicines, antihistamines or corticosteroids to reduce itchiness and swelling.
- Immunosuppressant drugs help regulate how your immune system functions.
- Light therapy to improve the appearance of your skin and remove blemishes.
- Avoid triggers that cause symptoms of eczema to flare up.
How do you treat childhood eczema?
If your child has skin issues, such as eczema, you can:
- Give your child a short, warm bath instead of a long, hot bath, which can dry out their skin.
- Use moisturizers several times daily. In infants with eczema, moisturizing on a regular basis, like with each diaper change, is extremely helpful.
- Keep the room temperature as regular as possible. Changes in room temperature and humidity can dry your child’s skin.
- Keep your child dressed in cotton. Wool, silk and synthetic fabrics such as polyester can irritate their skin.
- Use sensitive skin or unscented laundry detergent.
- Help your child avoid rubbing or scratching at their skin.
What type of moisturizer treats eczema?
There are several options of moisturizer available to treat eczema. Choose skin care products that:
- Are hypoallergenic, fragrance- and dye-free.
- Are gentle or for sensitive skin.
- Contain petroleum jelly or mineral oil.
- Don’t include preservatives or stabilizers.
- Have lipids and ceramides to improve your skin’s barrier.
It may take several different products through trial and error before you find one that works for you. If you need help choosing a moisturizer, talk to your healthcare provider.
How do I manage my eczema symptoms?
Treating and managing eczema can be difficult if the cause is something you can’t control, like genetics. Fortunately, you may have some influence over your environment and stress levels. Do your best to figure out what triggers or worsens your eczema, and then avoid it. The goal is to reduce itching and discomfort and prevent infection and additional flare-ups.
How soon after treatment will I feel better?
After treatment, it could take several weeks before your skin clears up completely. Topical medications or oral medications prescribed by your healthcare provider help your symptoms go away faster. If your symptoms get worse after treatment, or if they don’t clear up after a few weeks, contact your provider.
Are there complications from eczema?
Complications are possible with eczema and could include:
- Weeping eczema: Weeping eczema causes fluid-filled blisters to form on your skin.
- Infected eczema: Infected eczema occurs when bacteria, fungus or a virus breaks through your skin to cause an infection.
Symptoms that are a sign of complications include:
- Fever and chills.
- A clear to yellow fluid leaking out of blisters on your skin.
- Pain and swelling.
How can I prevent eczema?
There are steps you can take that may prevent eczema flare-ups and outbreaks, including:
- Moisturize your skin regularly or when your skin becomes dry. Seal in moisture after a bath or shower by immediately applying moisturizer to your skin.
- Take baths or showers with warm, not hot, water.
- Stay hydrated and drink at least eight glasses of water each day. Water helps keep your skin moist.
- Wear loose clothes made of cotton and other natural materials. Wash new clothing before wearing it. Avoid wool or synthetic fibers.
- Manage your stress and emotional triggers. See a psychiatrist for medication and a therapist for counseling if you’re experiencing symptoms of poor mental/emotional health.
- Use a humidifier if dry air makes your skin dry.
- Avoid irritants and allergens.
It’s important to note that eczema can be a complex and heterogeneous condition, and the specific causes and triggers can vary from person to person. Identifying and avoiding triggers, maintaining proper skin care, and using appropriate medications can help manage eczema effectively. If you or someone you know is experiencing symptoms of eczema, seeking medical advice from a healthcare professional or dermatologist is essential for proper diagnosis and management.